 Amy Wright |
Rapid Access Addiction Clinic breaks down barriers, offers immediate access to treatment
By: Jessica Lockhart
In an overburdened healthcare system, where emergency room visitors often lay in stretchers lining public hallways and millions of Canadians go without a family doctor, patients with addiction related concerns often fall to the bottom of the list when it comes both to priority and empathy.“There’s a tremendous amount of stigma and shame associated with addiction,” says Dr. Meldon Kahan, medical director of the Substance Use Service at Women’s College Hospital (WCH). “Patients are reluctant to disclose they have this problem because they know they may be treated with disdain, even by some healthcare professionals.”
But at a time when the number of opioid-related deaths in Ontario is skyrocketing — research has found one in six deaths among Ontarians aged 25 to 34 was related to opioids in 2015, a number that has likely increased in the years since — addictions treatment has taken on a new urgency.
To help address the crisis, WCH opened a Rapid Access Addiction Medicine (RAAM) clinic in the spring of 2017. It’s among the first barrier-free RAAM clinics in Toronto; patients addicted to opioids, alcohol or other drugs can see healthcare providers within one to two days, no pre-booked appointment or referral necessary, though referrals from family doctors, hospitals and community organizations are accepted.
The clinic is open on Monday, Tuesday and Thursday mornings and, since opening, has seen increasing numbers of patients come through its doors. In addition to improving access to addictions care in a destigmatized setting, the clinic is also working to address what Dr. Kahan sees as a systemic issue in the world of addictions treatment: an absence of a multipronged approach to care, where counselling and withdrawal treatment don’t have to be mutually exclusive.
“There’s a feeling in the healthcare system — among doctors, nurses, hospitals, primary care, and emergency departments — that addiction is not a healthcare issue. That it needs to be treated in specialized psychological centres,” Dr. Kahan says. “The addiction field reinforces that notion, so you have this weird split where you have these psychosocial treatment programs for alcohol, which don’t involve any anti-craving medications and where they view addiction as exclusively a psychological disease. And at the same time, you have these methadone clinics which view addiction exclusively as a matter of opiate withdrawal, and they give patients methadone with no other intervention.”
The RAAM clinic at WCH doesn’t subscribe solely to either method. Instead, it offers care driven simply by what each unique patient needs. The healthcare team will prescribe buprenorphine (known by the brand name Suboxone) to treat opiate addiction, medications to reduce alcohol cravings and other treatments for mild to moderate withdrawal, as well as solution focused psychosocial therapy, such as counselling and motivational interviewing. If needed, the clinic will also make referrals for psychiatry and for community services, such as structured counselling or group therapy, as well as connect patients with primary care.
“Substance use is a chronic condition. Like other chronic conditions, like diabetes or depression, patients need a multi-model approach,” says Irene Njoroge, advance practice nurse for the RAAM Clinic at Women’s College. “We need to support people facing addiction with the same support we give other patients with chronic health conditions.”
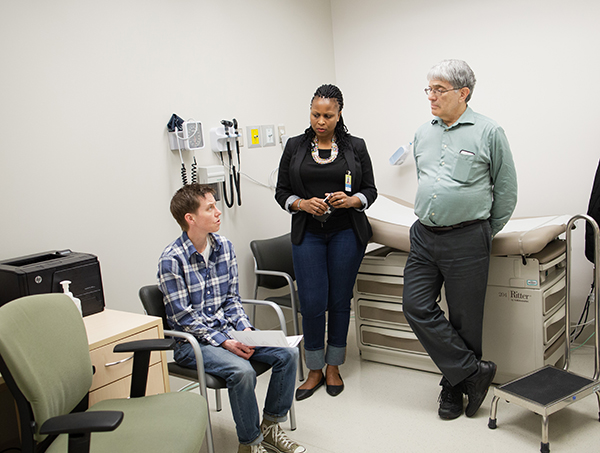
L-R: Amy Wright, Irene Njoroge, Dr. Meldon Kahan
Amy Wright, 41, works in community outreach at Toronto Public Health and is finishing up her master’s degree in social work at Ryerson University. She’s also a patient of the RAAM clinic. Wright visits the clinic to receive Suboxone, which she credits with helping her remain heroin-free for six-and-half years and counting. Wright uses Suboxone to help manage symptoms associated with colitis, for which she previously sought street opiates.
“When my colitis was still undiagnosed and when I would feel like I needed to use, I would still have to go buy a pill off the streets. Every time I’d have to go get a pill from the streets instead of going to the doctors, it really took a toll on my self-esteem,” Wright says. “It really made me feel like this awful person because I couldn’t go to the hospital like everyone else, or I couldn’t go to my doctor like everyone else and say, ‘This is going on. I’m in pain. Can you help me?’”
Now, Wright says, “If there’s a medical issue going on, I can go to the RAAM clinic.”
Like many people with substance-use issues, Wright’s descent into addiction began fairly innocuously. A years-long struggle with migraines intensified when, at 19, she began studies at York University. A prescription for painkillers eventually morphed into a reliance that would lead to her first overdose, and then her second and third, while she was still a university student. What she didn’t know was that she had undiagnosed depression; the drugs that treated her migraine pain also made her feel “more alive.”
Wright’s life, for the next decade or so, was marked by addiction driven by healthcare issues (fi bromyalgia, in addition to the migraines, colitis and depression) and brief periods of sobriety. There were more overdoses, both accidental and intentional, as well as periods of homelessness. By 2009, she found herself in Vancouver’s Downtown Eastside, where she spent a year and eight months using heroin, largely at a supervised clinic. It wasn’t until she learned that her brother, her only sibling, had taken his life that she found her motivation to return to Ontario and stop using; she detoxed on the cross-country Greyhound bus trip.
In the last few years, much of Wright’s work has focused on harm reduction, including helping design safe injection sites. Part of her current portfolio at Toronto Public Health is certifying and training people to use Naloxone. Rapid access is a model with proven results, both for patients and the system. By giving patients immediate access to care, rather than asking them to wait a week or more, their health outcomes are much better. “Withdrawal can often force even highly motivated patients to relapse,” says Njoroge.
“Being able to access these services when they need them is really serving them well.”
The model is also lessening the burden on the healthcare system, by reducing emergency department visits and engaging patients in both short- and long-term care. The WCH RAAM clinic is one of 12 current rapid-access clinics in the province. The initial seven clinics, opened in 2016, saved the healthcare system approximately $200,000 for the first 150 patients in their first 90 days of treatment.
“The program is improving access to evidence-based addictions treatment,” says Njoroge. “We are able to support the healthcare system to build capacity, and we’re improving care for patients with addictions. Traditionally there is a lot of stigma, a lot of shame and guilt, and in this model we are building the continuum of care.”
In Toronto, the program has supported the establishment of additional RAAM clinics at Sunnybrook Health Sciences Centre, Toronto Western Hospital and Michael Garron Hospital. The newest clinic is a partnership with the Anishnawbe Health Toronto and focuses on the healthcare needs of Indigenous people. The program has also partnered with the existing addiction clinics at St. Joseph’s Health Centre and St. Michael’s Hospital to integrate them with the rest of the Toronto RAAM network. Outside of Toronto, there are seven pilot sites across the province in London, Owen Sound, Ottawa, Newmarket, Sudbury, Sarnia and St. Catharines. Plans are in place to expand to community hospitals and to additional facilities across the province.
“We are very excited to see the tremendous success of the RAAM clinic that opened in Sudbury almost two-and-a-half years ago is now spreading across northern Ontario. With the opening of these northern RAAM clinics, patients in more remote areas will be able to access care close to their homes,” says Dr. Mike Franklyn, lead physician of the Sudbury RAAM. “Everyone, even the patients without a primary care provider, can now seek the type of specialized substance-use care they need that, prior to these RAAM clinics, simply did not exist. As a result, we’re seeing a decrease in ambulance and emergency room use, detox and also in hospital admissions that result from a single RAAM clinic visit.”




